“We do 12 to 14 deals a year and turn down 10 times that, so we’re doing 150 due diligences a year all over the world. “
https://www.strategy-business.com/article/Danahers-Instruments-of-Change?gko=6c075
“We do 12 to 14 deals a year and turn down 10 times that, so we’re doing 150 due diligences a year all over the world. “
https://www.strategy-business.com/article/Danahers-Instruments-of-Change?gko=6c075

Wait time: 61 days
time to avoid removal: 4.1 weeks remaining
Monday after May ‘2-4’ Long Weekend
On a call to Scotland speak with Prof Mackay in the morning, who mentioned he’s done 300 over 7 years. He was personable and his depth of knowledge on orthopedic practice far beyond any of the doctors I'd spoken to so far. He mentioned there are more professional football (a.k.a. soccer) & rugby players opting for this, also some pro skiers and skiers from the USA who traveled specifically to keep their ACL.
A consult could be scheduled as soon as Wednesday afternoon and surgery Friday. He suggested to plan at least 2 weeks there up to 6 weeks after, and to approach it like a vacation where I won’t be doing anything. It was also clarified when identified to be an InternalBrace candidate according to MRI (in previous post), a surgeon won’t know for sure until they’re inside the knee to examine the tissue, so depending on what he actually finds, a graft ACLreconstruction may turn out to be the best option, however he’s fairly optimistic; if needed we may do a hybrid: smaller graft & internal graft + keep ACL. For the ACL it depends on disruption of continuity.
An additional 20-30 min may be added to the procedure depending on the MCL (slight slack can move tension to ACL; spoke about the remodeling phase – laxity of system) and retention to natural length, so procedure may be 2-3 hours.
The timeline sensitivity was explained: preference for procedure is 3 – 6 weeks; we’re at 9. Briefly talks about some graft & stats on hamstring show some problems after.
Surgery will be somewhere called BMIRossHall in Glasgow Scotland. I’m fine with this,
I just want my sportsmedicine doctor to be giving me the option not to rip out healing body parts when it’s not needed, which isn’t happening in Canada. Or the USA. Or the UK.
timeline in pic
May 18, 2018
Saturday 2:27am
Mackay Office reply:
“I have forwarded this message to Professor Mackay, and for his advice on theatre availability.”
I settle in to wait the weekend. (won’t be skiing slushcup Sunshine village this year)
Monday is a Holiday in Canada however not in Scotland so I can follow up then.
My persistence may be paying off, thanks to David Hunt Tribe Medical , Peter from Gateway Surgical did contact me and suggested Jesse Shantz or Andrea Veljkovic are potential providers of current orthopedic practices in Canada; turns out they are also private – I contact them regardless, as the failure of the Canadian Healthcare system is not leaving an alternative.
The earliest option they have is an initial appointment for consultation Wed May 23 followed by surgery in Vancouver May 30. For some reason private healthcare is not allowed in Alberta, so to provide care patients have to fly to BC for the procedure. I would return right after, and they suggest I have food for a week or 2 & someone to help me while I’m healing & less mobile.
Some of my questions were for the surgeon so I wait to hear back from Jesse…
May 17, 2018
wait time: 58 days
time remaining to avoid removal: 4.4 weeks
I set my alarm for 2am, still pursuing every possible avenue – InternalBrace is my 1 window of opportunity – hoping to find a way I can do this without travel.

2:13am
The Mackey Clinic emails me the details they need, followed by a 2:27am email
“As per last email if you could provide your details, I will check theatre slots for you. So don’t worry about booking a consultation yourself.
In situations where a patient is traveling, as you are, the consultation, pre op assessment and surgery date – will be over 3 days usually. Are you able to travel at short notice ?”
3:56am
I reply
“I have the (MRI) pictures and am unable to open without PACS; Please let me know if you use the PACS system for viewing.
I am contacting Alberta Health tomorrow as they said this should not be a requirement.
Also, is it preferable to work on increasing range of motion in preparation for surgery ?
(currently it is stiff; MRI does not show retracted tissue; cannot straighten leg, have increased range to straighten >2.5cm. cannot bend all the way back - concerned bending may cause synovial fluid to erode any clot present)
Reviewing the studies on the Arthrex site, curious if this is still in trial phase stage - I'm still on board for it, just curious as the 2yr study results mentioned more results are needed.
Thank you, looking forward to this”
I’d been using a small stack of books below my #knee to push down to, and was removing them to gain range. It seemed exciting to make progress until I measured 2.5cm - which isn’t much.
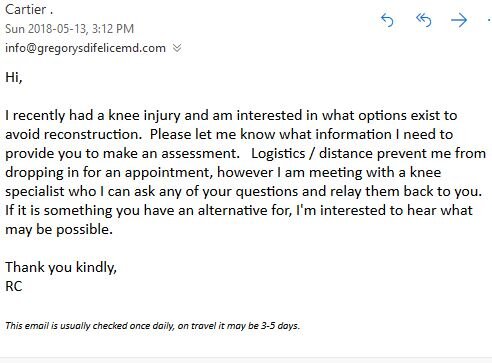
I also mentioned Dr Difelice and asked what other surgeons may provide current options.
6:38am
Mackay Office
“I would encourage early mobilisation as it will accelerate post op recovery. Logistically Greg Difelice would be easier to access, although we use different variations on the same technique. Although surgery is cheaper here, travel does add up.
I would normally encourage patients to take a 2 week vacation here before returning home, with DVT precautions – although there is still some associated risk.”
9:06 am
I send the requested info and reply “Travel on short notice is expected for this, let me know what the openings will be so I can work backwards and plan flights.”
Adding to my evaluation is the timeliness of having the procedure done which reports better outcomes the sooner it’s completed.

10:16am
I receive a reply from Tribe Medical to my email to find a rep Arthrex who can identify where this is offered in Canada
I look up Calgary orthopedic surgeons and am curious who is the most forward thinking that would be using current methods. Also figuring out how I can get the MRI report translated so I understand the technical / medical verbiage clearly. Searching what non-delineated ligament means…
Also the attenuation rate to determine how long I have.
23:57pm
I reply:
“Curious what you meant by different variations of the same technique; if they have names let me know I'll look them up - if too complicated we can discuss in consult.
I did a bit more digging and have identified a Jesse Shantz and Andrea (Andy) Veljkovic who can do this in Canada, however private health care is not allowed in Alberta so I have to fly regardless, in their case to Vancouver. Curious if you know them. I can ask what technique they use if this is important, or any other question you suggest. Depending on when we theatre availability in Scotland … they said they can provide some follow up in Calgary after, and earliest they could do procedure is May 30.
I'd like to have an idea of theatre dates and cost for procedure in #Scotland so I can calculate the exchange. I have no problem staying for at least 2 weeks as you suggested. Please let me know how time sensitive this is, and if May 30 is further off than desirable - if so it may be in my best interest to pursue a more expensive yet timely option to improve potential outcome.
I've figured out how to open the images, the program that does this is called Onis Viewer available free here:
http://www.onis-viewer.com/ProductInfo.aspx?id=19”
now I'm figuring out how to set up a 200Mb transfer to you.”
May 16 cont...
10:45
2nd AKIC U Calgary appointment (Finally)
.
Wait Time has been 57 days so far,
19 days behind actual scan completion
.
follow up to go over April 27 MRI results
Again, I feel reluctance to work with me, in only 2nd appointment. When I bring up ligamys doctor does not seem familiar with it and can't answer questions. I ask if he read the emails I sent with the information and am told they were not read.
.
.
I inform him the surgeon responded I may be an ideal candidate for InternalBrace and am told “We don’t do that here.” Concerned the help that could be offered on this will not be provided I said “I just need you to support which ever surgeon I end up working with by helping me get him the information he needs.” I do this to ensure consensus is established on how we’re going to proceed with expectations & responsibilities as I don’t know what may be required.
.
.
I told him I’d send the medical journal on Internal Brace to share & discuss with the surgeons so they know what I was referring to and how they can provide this option.
.
.
At this point I’m perplexed why they don’t know about this and am having some doubts about the Canadian Healthcare system.

1:46pm
I send the AKIC sportsmed doctor at U Calgary information on internal brace to share with the surgeons he had yet to tell me a name of, as I’ve lost faith they’re offering current practices however I don’t see why they wouldn’t be interested in learning practices with better patient outcomes. https://www.arthrex.com/what-surgeons-are-talking-about/131FD01B-7B44-491D-B5F7-015A9474A65E
2016 article on AHS from the Calgary Herald on MRI wait times increase in Calgary – how many of these could be understood by the work from my Aug 12 post:

Still eating fresh pineapple for bromelain, found in every part of the pineapple, but most plentiful in the stem. Seems the clot isn’t a concern anymore; pineapple enzyme is supposed to help break up existing clots and prevent future ones from forming. I usually blend it into a smoothie.
May 16, 2018
wait time: 57 days
time remaining to avoid removal: 4.5 weeks
.
Working on how I can get the MRI photos to display.
.
Just after midnight I follow up on the email I sent to Dr. Mackay, they reply after 4am. At 9am I let them know I’ll get the MRI pictures.
.

4:35am
Dr Mackay replies “It would appear that the InternalBrace could be ideal in this situation. It allows the ACL and MCL to repaired simultaneously if required.
.
If the ACL cannot be fully reconstituted it can be augmented with a reduced sized graft and backed up with the internal brace, reducing the #surgical insult. This approach also supports accelerated rehabilitation.”
.
I have a window.
.
I’m working in the morning so I try to get back to sleep each night as soon as I can.

8:43am
Follow up Dr Difelice with an email. I ended up calling at some point yesterday and they answered my questions. USA healthcare costs are WAY higher, not sure what problem is driving this for them (more on this later).
10am
I ask what else they need at the Mackay Clinic and what schedule provides the best possible outcome.
---------------
If you were like me with no prior knee injury knowledge, and read the same published articles, we'd share the foundation that an ACL regrows itself supported by multiple cases in different medical journals and other media, and over 110 surgeries; and be looking forward to your doctor going into more detail on this.
.
.
You also might assume the specialist advising you on potential courses of action to choose from - because it’s their field of expertise - will be able to further educate you on it.
This is the problem with assumptions and why one must validate them (beyond a Continuous Improvement event).
.
.
I didn’t receive the impression during the 1st appt my enthusiasm was shared when asking about alternatives to avoid unnecessarily removing a ligament that’s trying to heal or damaging good tissue to harvest a graft; nor did I receive replies to my specific questions in emails.
and the most recent thing I came across from last year:
Anterior Cruciate Ligament (ACL): Very Close To Human Trials
2017
https://www.rdmag.com/news/2017/11/how-close-are-scientists-regrowing-damaged-limbs
Dr. Cato Laurencin’s work in the previously uncharted territory of regrowing bones, tendons and ligaments.
the potential in the polymer technology for regrowing bones.
After successfully modeling how to regrow an ACL — which about 200,000 Americans injure each year — Laurencin has attempted the procedure in rabbits that he says are “running around and doing well.”
It has also been in one human patient who has had the regrown ACL for 3 years.
Laurencin says that he is now working with the U.S. Food and Drug Administration to start human trials.
Laurencin’s work regrowing ACLs was named one of the top scientific discoveries to change the world by National Geographic Magazine
so even if you’re a graft patient, looks like it’s only a matter of time before you can have your ACL back.
Which led me to search for this researchers more current work; here’s a publication:
World Journal of Orthopedics
2015
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4303781
“The worldwide estimation of young sports players that require surgery following a knee injury lies between 17%-61%. The anterior cruciate ligament (ACL), a main stabilizing structure of the knee, is one of the most commonly injured ligaments. In the USA alone, around 350,000 reconstructive surgeries of the ACL are performed annually. According to the National Center for Health Statistics, the annual costs for the acute care of these injuries are around $6 billion”
“relatively high failure rates of ACL reconstruction, especially in young and active patients, have been reported for allografts. An incidence of osteoarthritis as high as 50% within 7-14 years after injury and reconstruction of the ACL is still the main drawback of this surgical strategy. The development of osteoarthritis following ACL injury is not fully understood and may be caused not only by the limitation of the current grafts, but also by the initial joint trauma and the trauma caused by the surgeon.”
and the most recent thing I came across from last year next post…
I also came across the following
Aug 22, 2013
https://ctmirror.org/2013/08/22/uconn-scientist-working-new-way-repair-knees
There’s a clinical trial underway to test a new type of ligament Laurencin invented, which has already regenerated ACL tissue in animals. If successful, the next step would likely be a large clinical trial in the U.S. and seeking approval from the FDA to put the ligament into widespread use.
It’s part of the development of a field Laurencin calls regenerative engineering
Success of the surgery is often described in terms of how common it is for patients to return to sports; studies have offered varied pictures. Some have found 90% of patients return to sports 1 year after the surgery, others show the rate is closer to 50 - 70%.
In a patient with a torn ACL, the stump that remains contains a storehouse of nutrients and stemcells, which have the potential to grow into new tissue. Laurencin’s method involves using those cells and others that are already present, by placing a specially engineered “matrix” where the ligament should be. Cells can attach to it, creating new tissue.
“In many ways, we utilize the patient’s own body as a bioreactor, if you will, to be able to make the tissue,”
It took years to create the matrix, which had to have the right mechanical and chemical properties to allow for regeneration. Laurencin worked on it with James Cooper, a former PhD student now a prof at Rensselaer Polytechnic Institute in New York. The matrix, the L-C Ligament, is named for Laurencin and Cooper.
Research in rabbits showed that the matrix could regenerate an ACL. For the past 2 years, it was studied in sheep. The clinical trial in humans began in the Netherlands in June.
The L-C Ligament is designed to provide support for the knee as soon as it’s implanted. It takes between a year and 18 months to fully regenerate an ACL, Laurencin said.
The device was recently patented; patent-holder is Soft Tissue Regeneration, a New Haven-based co. Laurencin co-founded. The co. has received funding from the state’s Connecticut Innovations, which gives the state a share of the co.
I finally come across an article explaining what a grade 3 sprain is. (May help someone else trying to decipher this)
"About ½ of all injuries to the anterior cruciate ligament occur along with damage to other structures in the knee, such as articular cartilage, meniscus, or other ligaments.
Injured #ligaments are considered “sprains” and are graded on a severity scale.
Grade 1 Sprains
The ligament is mildly damaged in a Grade 1 Sprain. It has been slightly stretched, but is still able to help keep the knee joint stable.
Grade 2 Sprains
Stretches the ligament to the point where it becomes loose. This is often referred to as a partial tear of the ligament.
Grade 3 Sprains
This type of sprain is most commonly referred to as a complete tear of the ligament. The ligament has been split in 2 pieces, and the knee joint is unstable.
Partial tears of the ACL are rare;
More ACL injuries are complete or near complete #tears."
To better understand I pull out my #MRI again and reread (in Oct 6 & 7 posts).
2am
Reply from my DIS ligamys inquiry arrives, still 21 days, so not an option. Also received 5 more published papers on its results.

8am
I receive a reply from Canadian Research Ethics Board from my efforts to get an application in for BEAR Trial.

10:42am
I send the DIS published research to my Sports Medicine doctor at AKIC University of Calgary in preparation for my appointment 10am tomorrow. Is it strange to expect someone would be interested in their field of expertise?

11:09am
BEAR explains they are confused that I’m trying to both introduce their device to Canada, as well as be a patient.

12:27pm
I email BEAR again, and tell them I’m trying to both introduce their device to Canada, as well as be a patient.

3:07pm
BEAR trial let’s me know they won’t help even if I move to meet their 3 hour criteria. Still no criteria provided for me to pass on to my friend in the US.
I never ended up receiving a link from BEAR Trial to their 3rd trial criteria which I asked for several times to forward to a US friend.
I learn in addition to hospital funding, grant funding from the NFL (NFLPA player study harvard) was a significant factor in making BEAR trials possible. Curious if they are offering this to NFL players when they get injured.

8:52pm
I send the ultrasound to The Mackay Clinic, and inquire about my shortening timeline to avoid ACL attenuation, or other potential options to avoid removal if unnecessary. And maple syrup.
Found more info on internalbrace primary repair #surgical technique here:
https://www.arthrex.com/what-surgeons-are-talking-about/131FD01B-7B44-491D-B5F7-015A9474A65E
Despite the situation, I still had awesome #ski season, including the day this happened – even though this happened it was still a great day!
2:00am
Got up from 2am-4:30am Calgary time to reach Scotland at 9am UK time by phone, and then sent them info. Laughing because having a hard time to believe the absurdity that I actually need to call another country on this when the assumption is Canada has advanced healthcare.
2:44am
Just to be sure, I send an email asking if DIS / Ligamys is still limited to 21 days or if advances have been made where it can be done further out.


11:35am
I send an email to Dr. Mackay outlining my situation up till now - mentioning I’ve achieved an additional 2.5cm of range to straightening over the last week – and my appointment in 3 days.
Still grateful for my situation every time I see someone in worse shape than me.
The next report I came across really put the it into perspective the need for alternatives given complications and lower than toted outcomes of ACL reconstruction, and how InternalBrace initially measured up within the first 3 months – back in 2015.
Anterior Cruciate Ligament Repair Revisited. Preliminary Results of Primary Repair with Internal Brace Ligament Augmentation: A Case Series
“estimates suggest that in the United States alone 400,000 ACL reconstructions are carried out each year. As the majority of ACL injuries occur in patients of working age, the economic burden to both patients and society is considerable”
“ACL reconstruction. The technique either involves removing or bypassing residual ACL tissue, without any attempt to repair the ligament”
“In the majority of cases, sufficient tissue remains for a repair to be considered, particularly if surgery is carried out within 6 weeks of injury”
*What really strikes me – perhaps from my continuous improvement background – is removal & reconstruction is a work around to the problem*
“A number of problems have been identified with ACL removal however, with autograft harvest associated with a degree of morbidity from tissue loss. Hamstring muscle weakness following harvesting averages 10% in most studies with anterior knee pain common with patellar tendon grafts”
“loss of proprioception a particular problem. Not surprisingly therefore the majority of studies of gait after ACL reconstruction show abnormal gait patterns and altered knee kinematics which may be linked to the higher rate of early Osteoarthritis”

Orthopedic & Muscular System: Current Research ISSN:2161-0533
“68 consecutive patients who underwent Anterior Cruciate Ligament repair with IBLA were followed for a minimum of 1 year following #surgery … between Sept 2011 and Sept 2014”
“Only patients who had completed one year of follow-up were included … max time from injury to surgery was increased to 3 months”
*I’m within this time frame, & receiving a diagnosis that will not facilitate a successful outcome*
“Beyond this time the ACL remnant begins to remodel and retract, and the tissue is no longer able to be placed back at its original attachment point”
“Loss of proprioception is important as it may lead to overloading of the ACL graft ... It is estimated that less than 50% of patients return to sport after reconstruction, and those that do often find that they cannot perform at the same level as pre-injury/pre-surgery”
“The majority of studies assessing gait and knee kinematics post-ACL reconstruction show an improvement in gait pattern compared to pre-surgery, but compensatory mechanisms of muscle use persist in the majority of patients indicating sub-optimal performance of the reconstructed graft. Graft donor site morbidity from tissue loss and scarring is well documented with hamstring weakness and anterior knee pain problematic after hamstring and patellar tendon harvesting respectively”
“modifications introduced to the ACL reconstruction technique to try to improve outcomes include: changes in graft tunnel position, double bundle rather than single bundle grafts, retention of the ACL remnant and variations in graft fixation techniques.
NONE of these modifications have been shown to make a significant difference to patient reported outcomes.”
*Earlier return to function could result in less hospitalisation and healthcare usage post-operatively, with an earlier return to work and sport. This could potentially have benefits not only to the patient but to the health service and society as a whole.
the time to surgery in patients undergoing acute ACL repair with IBLA is likely to be shorter than those undergoing ACL removals, the majority of whom will have failed a period of conservative care.

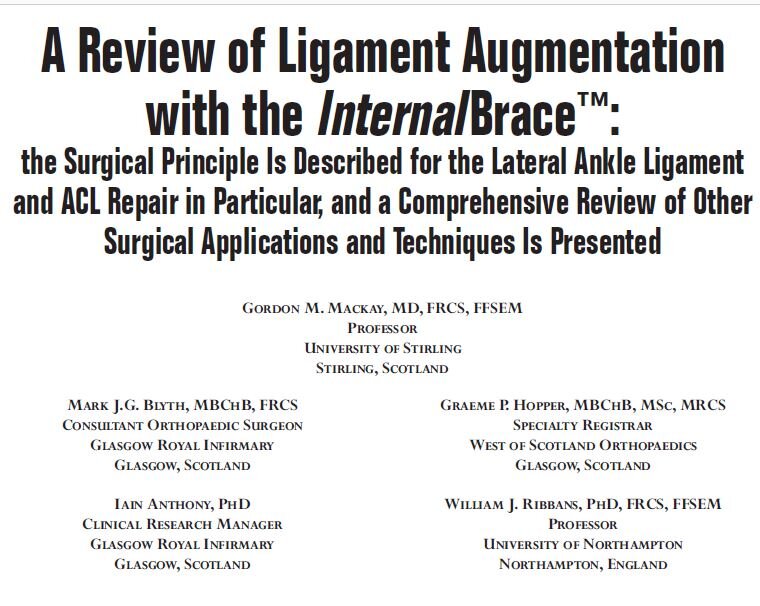
One of the names I noticed on a few publications was Dr. Mackay at The Mackay Clinic, who it turns out pioneered the InternalBrace, and found the following:
“2 International Netball players have regained pre-injury levels of function 12 weeks after their ACL rupture has been treated with the internal brace.
“with the healing of their ACL confirmed by MRI. These exceptional outcomes are partly explained by the procedure’s preservation of nerve and blood supply and the avoidance of donor site problems thanks to the IB fixation, although the duration of recovery is also determined by the individual and the unique nature of their injury. The Internal Brace is quickly becoming a standard procedure in skiing and impact sports, especially in the USA,”
https://www.mackayclinic.co.uk/the-internal-brace-at-a-glance
I started looking up everything I could find on this, so I could talk about having it done here during my next appointment this week at AKIC with my sports medicine doctor at University of Calgary.
Side note related to stairs - I also recall a meeting to explore a possible Operations Manager position with a fast growing startup May 2nd. They had stairs and I hoped they didn't ask me to walk up them to where the offices are – stairs were very difficult at this point – luckily we had it in the main area which was a nice change. Still tried to make it less obvious.
Despite the timeline passing for DIS eligibility, the fact a repair option regrowing ACL’s has existed for so long spurred me to keep looking.
I came across article A Review of Ligament Augmentation with the InternalBrace
Halfway through the 18 pages I find some application to the ACL, how it reduces harvest site morbidity & cost.
Based on the US stat 1 – 10 per 1000 people = 100k – 400k ACL reconstruction s occur annually; Canada would have 32,000+ reconstructions, which involves removing or bypassing the remaining ACL, despite in the majority of cases sufficient tissue remains for a repair to be considered, particularly within 3 months.
It explained grafts do not produce a normal feeling knee; there’s a loss of proprioception, which when present is important as this prevents overloading of the ACL graft; and estimates less than 50% of patients return to sport, and those that do often find they cannot perform at the same level.
“Graft harvest is associated with a degree of morbidity from tissue loss; muscle weakness with hamstring grafts & anterior knee pain are common with patellar tendon grafts.”
“there is a decrease in knee power and work performed postoperatively by the muscles around the injured knee”
“compensatory mechanisms of muscle use persist in the majority of patients, indicating sub optimal performance of the reconstructed graft”
There was also a study cited confirming “significant increase in osteoarthritic changes as early as a year post op” and stats on reconstruction failures.
“The clinical benefits of a well prepared and healed ACL are likely to be greater for patients than those offered by a traditional ACL reconstruction”
“Sufficient ACL tissue can remain for up to 3 months following ACL injury to allow a repair; procedure is time dependent as the ACL remnants are not suitable for direct repair after the tissue retracts and atrophies”
Perhaps this is an option I am still within the timeline for. I have just under 5 weeks left if it is.
The Internal Brace is a 2mm high molecular weight polyethylene that protects a repair by being a check rein if the ligament is stretched beyond its physiological range. Should failure occur reconstruction remains possible without compromise to the knee joint.
Earliest patients are from Sept. 2011
If found suitable, the ability to repair a torn ACL can be confirmed at the time of #surgery.
“Early phase rehabilitation was consistently accelerated. Limited pain and selling facilitated early range of movement, muscle control and restoration of function.”
“…avoidance of donor site morbidity & minimal surgical trauma.”
“better outcomes were achieved for ACL repair at the majority of time points”
“Pain…was less in patients”
“4 cases had arthroscopically confirmed ACL healing”
“…eliminate the shortcoming of current reconstruction techniques”
“…change in orthopaedic practice relegating ligament reconstruction appropriately as a salvage procedure; only if the tissues fail to heal adequately after augmentation & repair.”
The article is from back in 2015, so I start searching the authors of the published medical journal studies and references to find other research they’ve done.
May 13, 2018
53 days since injury.
I come across some info on ALL (Anterolateral Ligament) and find:
‘Despite technologic advances in the surgical technique for ACL reconstruction, some patients continue to have rotational instability post operatively, decreasing the return to sport rate. Failures can occur because of improper tunnel positioning, problems with patient rehabilitation, or non-optimal incorporation of the graft used for reconstruction’
and
‘recent biomechanical studies have shown it is an important stabilizer against anterolateral tibial rotation’
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5263705
Then found in Dr DiFelice NY’s article
Ground Breaking ACL Repair Approach Could Help 80,000 in US Alone
“Skier Veronika Velez Zuzulova competed 20 weeks after suffering a torn right ACL: an injury that according to traditional thinking should have required ACL Reconstruction Surgery and an 8 - 12 month #recovery.
Foregoing the traditional, Zuzulova opted for ground breaking ACL repair surgery instead of ACL removal & graft reconstruction – that had her training just 6 weeks after surgery with enough time to enable her to be ready for the Pyeong Chang Olympic Games.”
“more than 150 Repairs and has published both two-year and five-year post-surgery data on his initial cohort to validate the procedure’s success”
“published more than 15 professional, peer-reviewed articles on the subject”
“unwarranted bias which limited ACL Repair as an option”
“failing to recognize that ACL Repair success was much higher when treating specific types of tears, the data lead to the erroneous conclusion that ACL Repair was not a reliable course of action.”
Can “repair greater than 50% of the athletes who present to him with ACL tear”
“up to 80,000 of the 300,000 patients suffering ACL tears in the US alone may be helped”
French surgeon Dr. Bertrand Sonnery Cottet performed Zuzulova’s surgery, and again the article mentioned Scotland's Dr. Gordon MacKay at The Mackay Clinic.
Despite the mounting cases and supporting publications suggesting that, for the appropriate tear type, ACL Repair is the preferred treatment method, the shift away from unnecessary reconstructions —widely ascribed to by orthopaedic surgeons—has been slow.
"To keep all options open, athletes, parents and healthcare professionals need to take a closer look at ACL Repair," says Dr. Gregory S. DiFelice. This is especially important for younger athletes who have been shown to have high rates of re-injury and can develop significant arthritic changes as early as 10 years post-reconstruction.
"success rate with ACL Repair is approximately 95% in all comers from recreational up to professional athletes. In the few patients that have suffered re-injury, Reconstruction was performed without undue difficulties. It is interesting to note that Dr DiFelice uses the standard Reconstruction procedure only as the last resort whereas the majority of #surgeons use it as their only option."
https://www.gregorysdifelicemd.com/olympic-skier-miracle-comeback.html
Analysis of the older data reveals certain subgroups, especially proximal tears with good tissue quality, had better outcomes.
Again, the acuteness of the tear was a significant factor in repair – it is quite clear the direction I was being in given in Canada was wrong, and reducing the likelihood of a positive outcome.
I email Dr Difelice to find out what I can ask at my appointment this week, and am prepared to go to the US again.

Also email DIS again. Ensuring I exhaust all potential options.

Prior to the brace I noticed people look at me more; seems the limp was really noticeable. They still look at me with the brace too.
May 5, 2018
Also found another article on ACL Regeneration, this time in an 8 year old with mid-substance rupture, where "conservative treatment with a brace led to a stable knee with regeneration of the ACL on both the physical examination and MRI after 5 years."
https://www.rpajanssen.nl/images/user/files/JKSR%20ACL%20healing.pdf

I email my doctor one of the articles, asking for information on the % of ACL tear, and confirmation whether clot retention is needed to facilitate ligament healing, and if the bending exercises they prescribed will work against the bodies natural healing mechanism. I stop doing the exercises pending response.
May 6, 2018
Bent my leg while I was sleeping, pain returns.
No reply from email yesterday.

Some obvious signs I maintained my sense of humour through this;
something my friend found on their bike she found funny:

There was also a day in the week it was raining & I walked across a gravel parking lot on my way home from work; found out it was muddy & very slippy - which would have never been an issue before - however with limited range of motion quickly became the slowest & most treacherous walk I may have had.

While all this has been going on, I haven’t missed a day of work & continue adapting to function. There’s a noticeable difference in the way people look at me with a disability – in public I find they spend more time looking at me, perhaps trying to figure what’s different. Perhaps we all blend in until a disability is visible which catches people’s attention and they try to figure it out. One benefit is this will deepen my empathy.
People have also been helpful opening doors when they notice this which I’m thankful for.
May 1, 2018
While on the call, the doctor recommended I wear a brace for this injury – which I think is funny, as apparently I haven’t needed one for the last 45 days since it happened I’ve been waiting for diagnosis. He recommends getting one at Colman Prosthetics & Orthotics. So I contact them and they say I need to provide them a prescription.
May 2, 2018
I call the doctor’s office and request he write a prescription for the knee brace he recommended.
May 3, 2018
I pick up the prescription from AKIC at the University of Calgary and drop it Colman Prosthetics

May 4, 2018
Get fitted for an Ossur GII Rehab knee brace.
Found these instructions online, hopefully they help someone:

A lot of running around over 4 days that would be quickly identified and addressed through lean healthcare, saving time for the patient, doctor & prosthetic supplier. Let’s start

I also sent an inquiry to the BEAR Trial team on how this can be available in Canada (see pic).
They responded it is still in research phase, so I asked how to get it into research phase in Canada as well.

I followed this with a request for the BEAR III Trial criteria & details, as I learned the 100 BEAR Trial 2 outcomes were so strong a further round of 100 is proceeding with surgery to save ACLs.